

Focus on caregivers
[May 2021] BPCE L’Observatoire recently published research into the role played by family caregivers looking after infirm, elderly or disabled relatives. Who are these caregivers? What kind of ecosystem is set up around the people receiving care? Money-related issues are omnipresent but frequently remain taboo...


Although far from being a new phenomenon, the role of family caregivers has gained prominence in public debate in recent years, emerging from the intimacy of the home where it had long remained hidden. In the light of future demographic changes, the difficult financial balancing act involved in responding to diminished autonomy, etc., it is clear that the essential role played by caregivers – whose importance has been brought into stark relief by the health crisis triggered by the Covid-19 epidemic – is destined to expand and evolve in the years to come. BPCE L’Observatoire presents its initial findings in this area on the basis of two original and open-minded surveys conducted at the end of 2020.
15 million caregivers
Caregivers are not a social category per se but rather a heterogeneous group of people facing the same experience of supporting a loved one.
According to the definition used in the BPCE study, 29% of French people over the age of 15 are caregivers, equal to a total of roughly 15 million people. In addition to these caregivers, 9% are ‘occasional caregivers,’ i.e. people taking care of a loved one for less than three hours or less than once a week, and 19% are former caregivers. In total, 57% of the French are, or have been, caregivers to varying degrees.


[Définition] A CAREGIVER is any (non-professional) person who provides assistance to a loved one experiencing difficulties in his or her daily life owing to infirmity, disability or old age. It may take the form of assistance in daily life acts, or material, financial or moral support. This assistance is provided at least once a week and for at least three hours weekly.
The sheer scale of this phenomenon affecting virtually all categories of the population has resulted in a greater collective awareness of this problem, and even to a form of social and political recognition. The national mobilization and support strategy for caregivers launched in October 2019 is one example of this heightened awareness, an initiative welcomed by caregivers (83% of whom see these measures in a positive light) just like the greater commitment expressed by employers in this area. The mobilization of association networks, whose support and advocacy actions in favor of caregivers have been stepped up over the past decade, also plays a key role in this shift in perception, taking caregiving out of the private and into the collective realm.
73% of caregivers also hold down jobs
76% of French people say they have already heard about the notion of ‘caregiver’
A veritable ecosystem created around care recipients
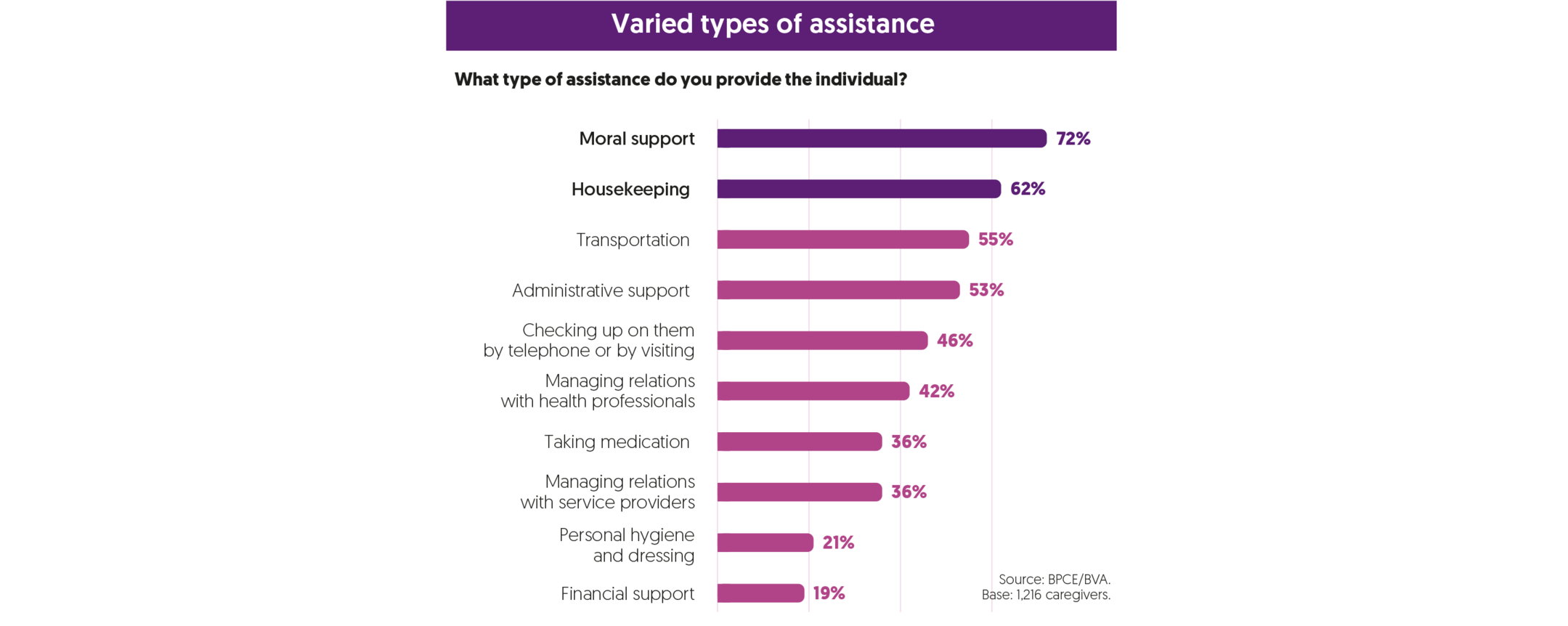
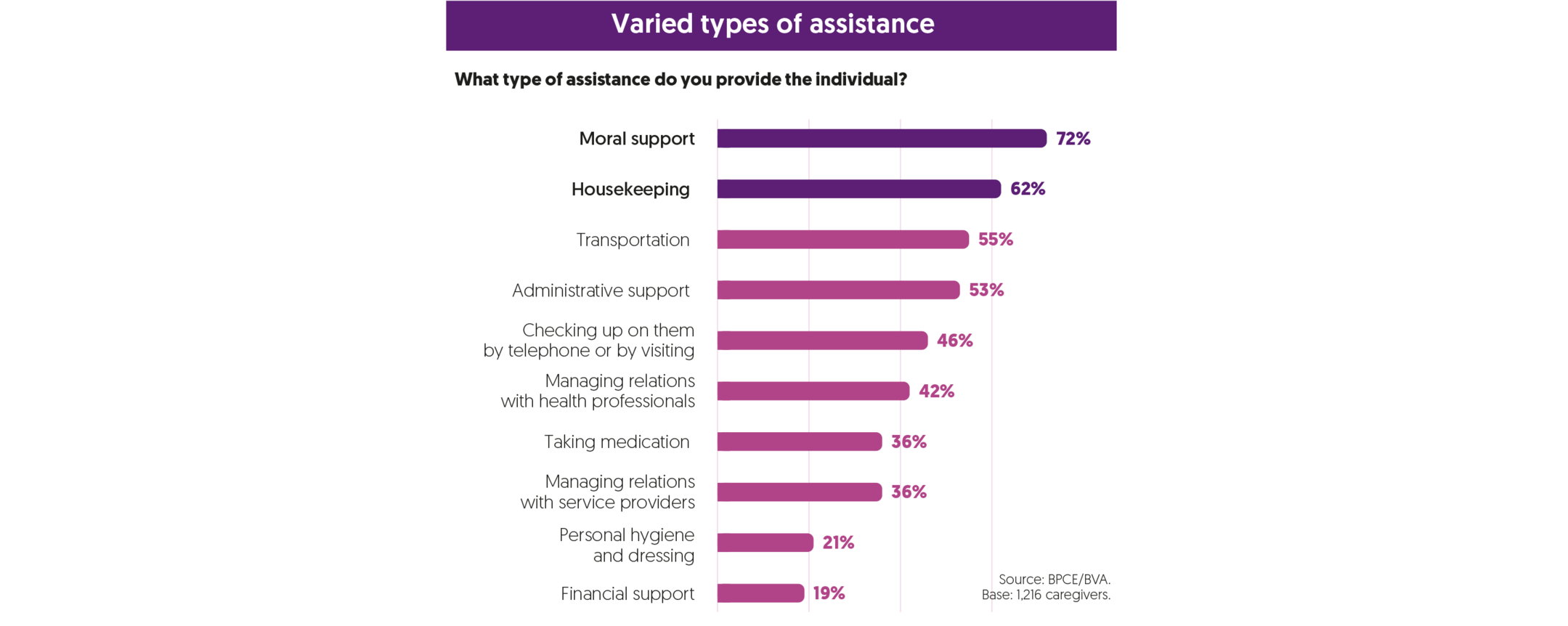
There exists an average of 1.9 caregivers for one person receiving care. More than half of caregivers (54%) say that they carry out their duties alongside other caregivers, while 46% state that they do it alone. Professional care providers are present in the recipient’s home in 56% of cases, an assistance that is by no means easy to obtain.
It is clear that being able to count on third-party support, whether from other family caregivers or professionals, is a key advantage to avoid the risk of feeling isolated, of social withdrawal or exhaustion encountered by many caregivers. And yet, an analysis of caregiver ecosystems overall reveals that they rarely function at optimal efficiency owing to an imbalance in how the burden is shared between caregivers, difficulties in day-to-day organization, open or latent conflicts within the circle of family and friends, etc.
The decision-making process itself is extremely complex, particularly when difficult decisions must be made that deeply affect the person receiving care, such as being transferred into a specialized institution
Money: a taboo subject… yet constantly omnipresent
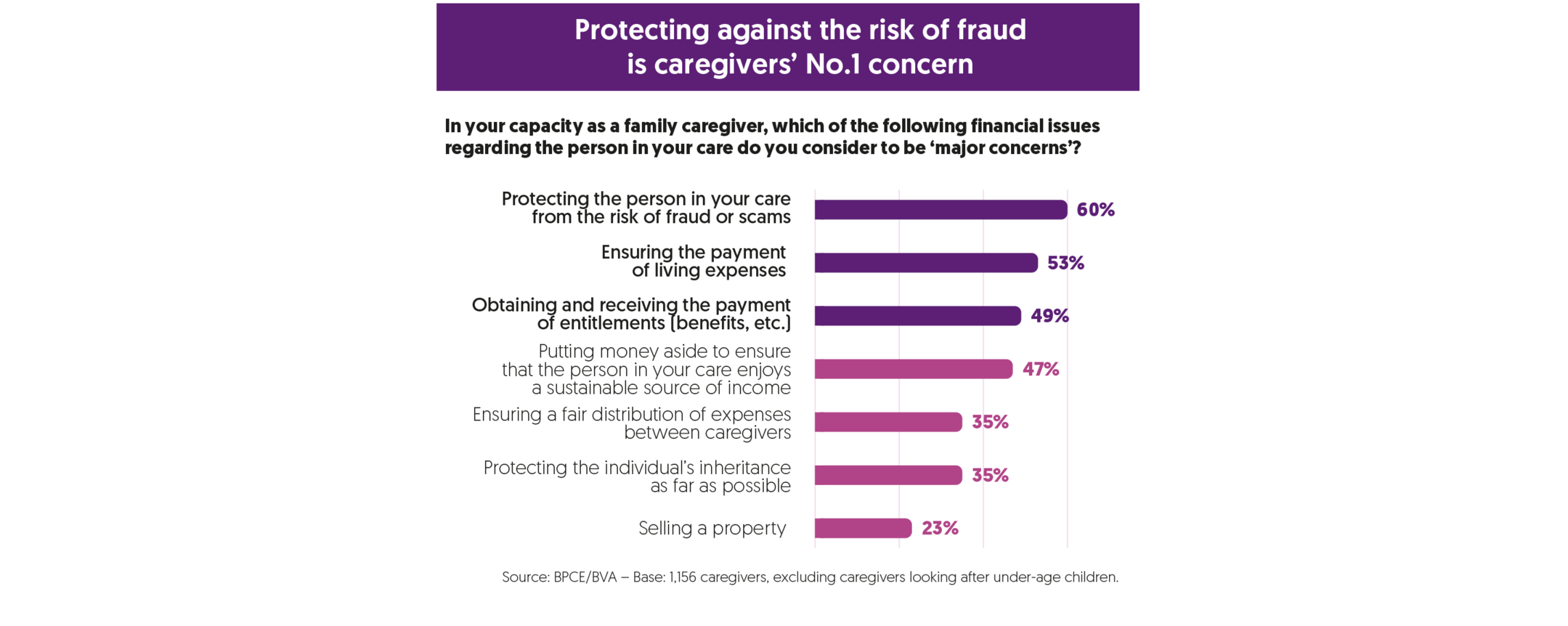
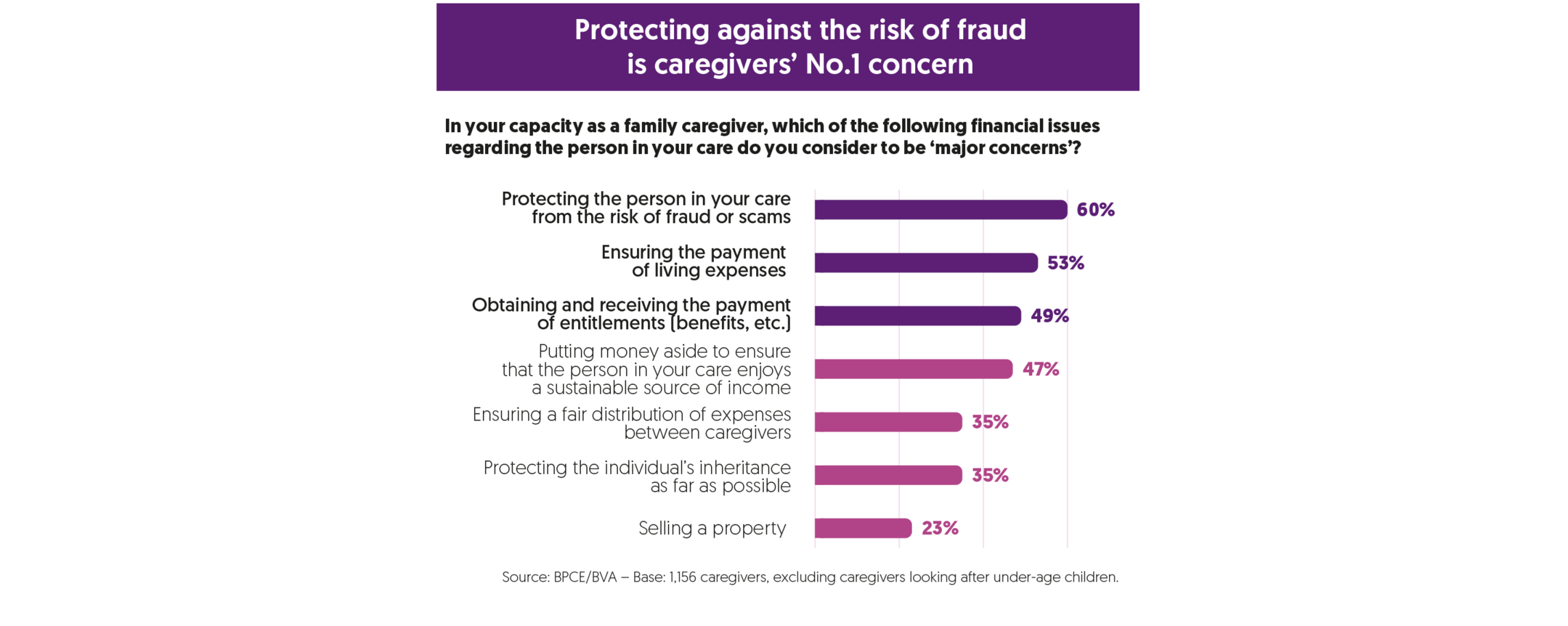
Money-related issues are acutely present, yet their importance is underestimated more often than not. These questions assume multiple forms: meeting the cost of expenses or paying excess health-care charges, managing the budget and accounts on a daily basis, remaining vigilant about the risk of fraud or scams, mobilizing assets, etc.
While 70% of caregivers consider the financial situation of the person in their care to be ‘good,’ personal financial dealings between the caregiver and care recipient are relatively frequent: according to our survey, 59% of caregivers settle expenses or provide the person in their care with financial support; 27% do so on a regular basis, and 32% more occasionally. This help most frequently covers small daily expenses but it can, at times, be for more substantial amounts: for 30% of caregivers, this financial assistance comes to more than 250 euros per month. The foreseeable decline in the standard of living enjoyed by pensioners – by 15% or 20% between now and 2050 – could be partially offset by caregivers and lead to an increase in the size of these cash transfers, raising the crucial question of how the financial burden should be shared between people suffering from diminished autonomy, their caregivers, and the wider community.
59% of caregivers cover expenses or give financial support to the person in their care
Our findings show that 71% of caregivers are involved in monitoring or managing accounts on a day-to-day basis but this is frequently done in an informal capacity, potentially creating a source of legal risks and conflicts. Moreover, while 83% of the care recipients possess assets, only 26% of caregivers are involved in managing them on a regular basis.
The omnipresence of money-related issues stands in contrast with the virtual absence of ‘real’ discussions about the individual’s finances. Sensitive subjects, such as the mobilization of assets and the sale of the principal residence or the adoption of legal protection measures, are poorly anticipated, leading to decisions being made in a rush and under poor conditions.
A typology of caregivers
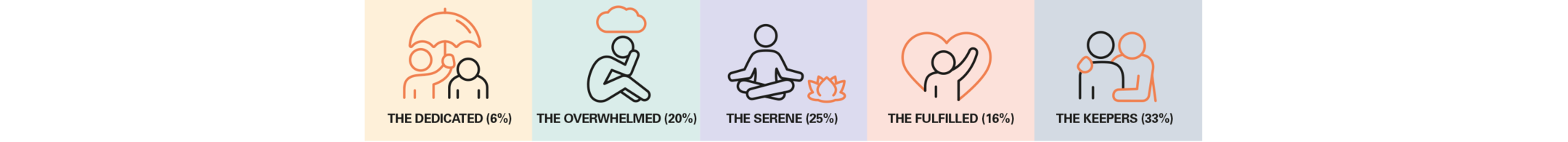
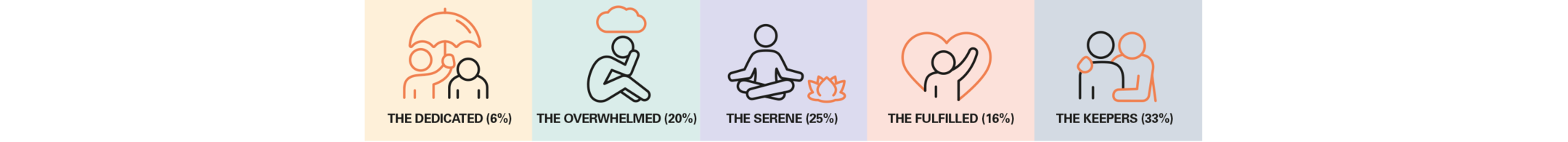
Paradoxically, caregivers generally describe their experience in positive terms despite mentioning major difficulties in carrying out their responsibilities, with the mental workload being the most frequently cited. Behind this observation, there emerge several extremely heterogeneous situations. Our research offers a typology based on five different groups that can be distinguished in three main ways: the intensity of the care provided, the assessment of the caregivers’ lived experience, and financial issues.
- The Dedicated (6%) devote themselves almost full-time to the care of their loved one, frequently a child or a spouse, with a positive experience rooted in the emotional relationship.
- The Overwhelmed (20%) are the most at-risk group: they are caregivers, often women, who find their situation very difficult to endure suffering, as they do, from a sense of powerlessness and a heavy mental burden exacerbated by a lack of financial resources.
- The Serene (25%) have achieved a successful balance, despite the – at times – severely diminished autonomy of their loved one, thanks to strong relational and financial resources and to the more frequent use of professional help; these caregivers are more frequently men holding down jobs, notably in managerial positions; their experience is positive.
- The Fulfilled (16%) are caregivers who enjoy the most positive experience, buoyed up by a sense of being useful, or even by a sense of pride in what they are doing; their commitment is more often chosen than imposed: they support a loved one from outside the immediate family circle (grandparent, friend, etc.) and/or whose disability is moderate in nature.
- The Keepers (33%) accompany a very elderly relative (the average age of the people receiving care is 75), mainly through more occasional supervision; the lived experience of people in this category is mixed because the caregivers, who are elderly themselves, wonder about what will happen as they grow older.
This typology underlines the sheer diversity of caregivers’ needs, all the more so as these needs evolve considerably over the caregivers’ lives. Being a caregiver is a long-term commitment: the individuals included in the survey have been caregivers for an average of 5 years while 15% have been providing care for more than ten years.
These findings call for an open and pragmatic approach. The challenge is not so much to define caregivers – that is the possible danger of creating an official ‘caregiver’ status – as to create an ecosystem of players and mechanisms capable of embracing this diversity of circumstances and of identifying the most at-risk situations. We also need to provide a better response to the transversal needs identified in the ‘BPCE L’Observatoire – Caregivers’ report, namely: mediation, externalization, and anticipation, notably as far as money-related issues are concerned.
For further details: (French only)
[In French only] BPCE L’Observatoire “Le temps des aidants” (avril 2021)
DOCUMENT PDF – 4,9 MB
Consult here the studies published by BPCE’s experts on caregivers:
To watch this YouTube video, you must accept cookies from the Social Networks category, which includes YouTube, by clicking here.

Interview with Sophie Cluzel, Secretary of State attached to the French Prime Minister responsible for the disabled
Sophie Cluzel, Secretary of State attached to the French Prime Minister responsible for the disabled, inaugurated the press conference convened to present the BPCE L’Observatoire report on caregivers.

